Why Evidence-Based Practice Matters in Mental Health Technology
At Precise Behavioral, being clinician-owned means two things: literally, our CEO is a working psychiatrist and remains active in the field of treating patients; and more broadly, we are grounded in safety, integrity, and quality across everything we build. One of our guiding principles is the use of evidence-based approaches. Not just in clinical care, but also in the digital mental health solutions we design.
It’s a term you hear often in healthcare: evidence-based. But what does it really mean, and why is it so critical when it comes to online mental health counseling and other technology-enabled care?
Why “Evidence-Based” Is More Than a Buzzword
In the expansive digital health marketplace, many products describe themselves as “evidence-based.” Sometimes it’s used as a marketing term, implying scientific legitimacy without actually being backed by research. But in clinical practice, evidence-based is not a slogan. It is a standard that we hold each other to when treating patients face-to-face, and the same standard guides us as we develop digital solutions to meet mental health care needs.
The real meaning goes far beyond sounding scientific. It reflects a rigorous process of research, testing, and validation to ensure that an approach is not only effective but also safe and adaptable across diverse populations.
Defining Evidence-Based Practice (EBP)
The American Psychological Association (APA) defines evidence-based practice in psychology as “the integration of the best available research with clinical expertise in the context of patient characteristics, culture, and preferences” (APA, 2006).
This definition highlights three essential components:
- Research Evidence – Clinical trials and peer-reviewed studies confirm that the approach works.
- Clinical Expertise – The judgment and experience of qualified clinicians guide how the method is applied.
- Patient Values – Individual needs, backgrounds, and preferences shape how care is delivered.
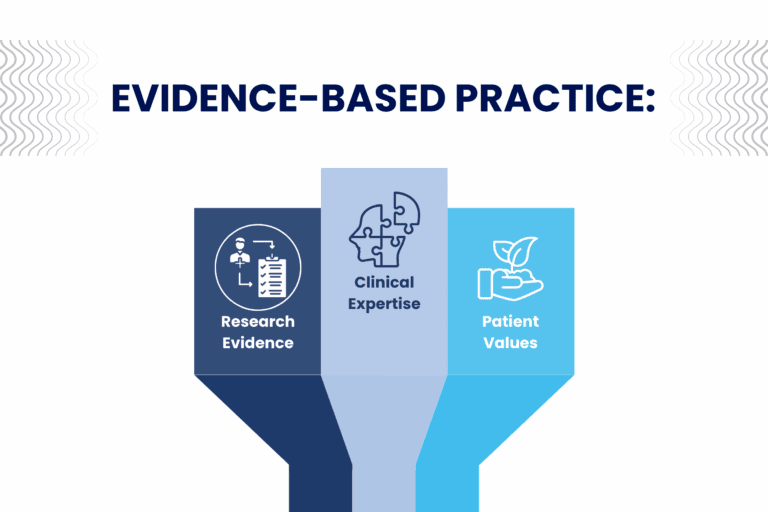
When all three elements come together, you have an approach that is not only scientifically valid but also personalized, ethical, and practical—whether in person or through telehealth counseling.
Why EBP Matters in Mental Health
The first rule of medicine has always been: do no harm. In mental health, where treatment often finds people during their most difficult moments, this principle is especially important. Interventions that lack an evidence base can worsen symptoms, delay proper treatment, or erode trust in care.
By contrast, evidence-based practices are repeatedly shown to produce positive outcomes across age groups, genders, and cultures. They provide a safeguard against harm and a roadmap for achieving real, measurable improvements in people’s lives.
At Precise Behavioral, we see our role as both innovators and advocates of this standard. Our goal is not to reinvent mental health care from scratch, but to build upon proven methods and expand their reach through technology.
Translating EBP Into Technology
One of the most exciting opportunities in mental health today is the ability to bring evidence-based care into digital formats. By digitizing proven approaches such as Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and mindfulness practices, we can help patients access support whenever and wherever they need it.
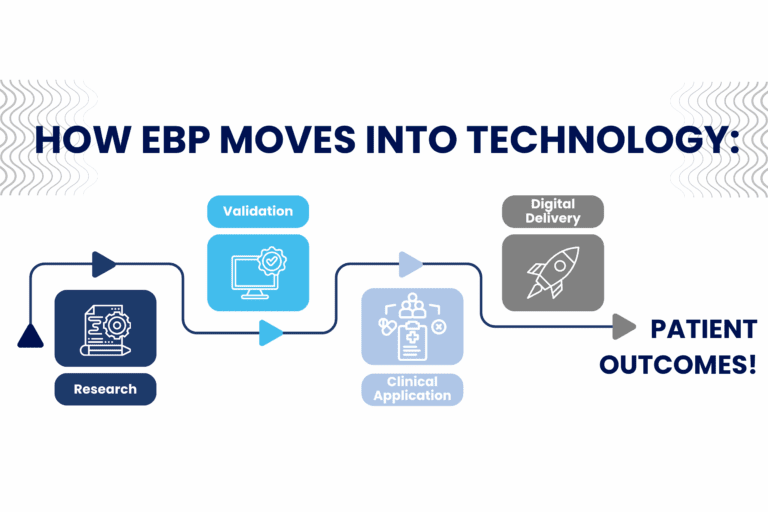
Research, for example, has shown that digital CBT programs can significantly reduce symptoms of depression and anxiety, often with results comparable to in-person therapy (Carlbring et al., 2018). These solutions are not just convenient: they are effective, scalable, and often more accessible to individuals who otherwise face barriers to care.
At Precise Behavioral, we integrate these validated methods into our platforms. Doing so maintains consistency with the care patients receive from their clinicians. This alignment ensures that patients experience a seamless continuum of support, whether they are in a therapy session, waiting for an appointment, using our tools independently, or receiving outside care that also has a standard of EBP.
Our Commitment
In mental health care, evidence-based practice is not optional. It is the ethical, effective foundation for everything we do. Without it, digital solutions risk becoming shiny on the surface but hollow products that fail the very people they are meant to serve.
At Precise Behavioral, our clinician-led perspective ensures that every product we build honors the research, safeguards patient well-being, and drives measurable outcomes. Evidence-based practice isn’t just part of our work; it is our work. By embedding it into everything from online behavioral health platforms to post-discharge behavioral health follow-up, we help ensure patients receive consistent, high-quality care no matter the setting.
And as we continue developing digital tools to close the gaps in mental health care, one thing will never change: our commitment to grounding every solution in the practices proven to help people heal, grow, and thrive.
References:
- American Psychological Association. (2006). Evidence-based practice in psychology. American Psychologist, 61(4), 271–285. https://doi.org/10.1037/0003-066X.61.4.271
- Andersson, G., & Titov, N. (2014). Advantages and limitations of Internet-based interventions for common mental disorders. World Psychiatry, 13(1), 4–11. https://doi.org/10.1002/wps.20083
- Carlbring, P., Andersson, G., Cuijpers, P., Riper, H., & Hedman-Lagerlöf, E. (2018). Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: An updated systematic review and meta-analysis. Cognitive Behaviour Therapy, 47(1), 1–18. https://doi.org/10.1080/16506073.2017.1401115
- Firth, J., Torous, J., Nicholas, J., Carney, R., Rosenbaum, S., & Sarris, J. (2017). Can smartphone mental health interventions reduce symptoms of anxiety? A meta-analysis of randomized controlled trials. Journal of Affective Disorders, 218, 15–22. https://doi.org/10.1016/j.jad.2017.04.046
- Torous, J., & Roberts, L. W. (2017). Needed innovation in digital health and smartphone applications for mental health: Transparency and trust. JAMA Psychiatry, 74(5), 437–438. https://doi.org/10.1001/jamapsychiatry.2017.0262
Written by Emily Yi
About the Author
Emily is a Behavioral Health Consultant at Precise Behavioral, Inc., and a Licensed Clinical Social Worker (LCSW). She specializes in supporting emotionally intense teens, adults, and families through creative therapy.
Editorial Contributors
This piece was edited by Greta Baker.



